The Effect of 3D-Printing Proximal Tibia Fractures in Preoperative Planning
Authors: Viberg B, Damborg FL, Rotwitt L, Jordy A, Holte MB & Gundtoft PH
In: Program & Abstracts from DOS Congress 2020; 168:189
Link: DOS Congress 2020
Abstract
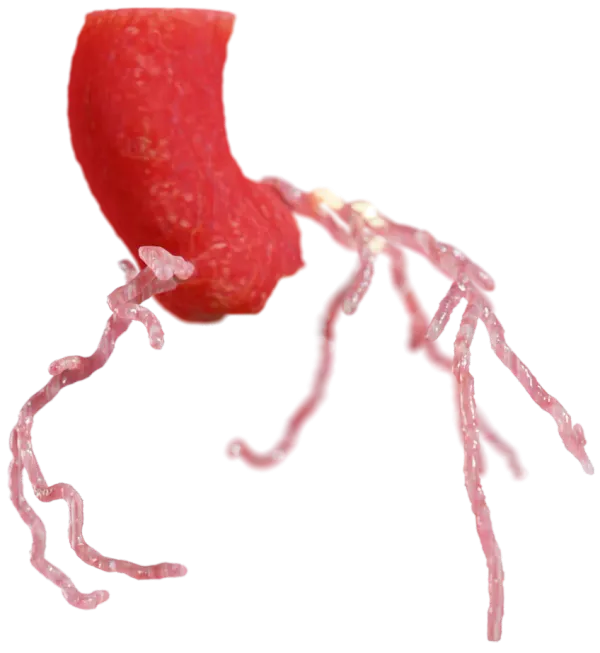
Background: 3D-printing of bones is novel way in preoperative planning giving the surgeon a real-size fracture to evaluate by hand. There are studies from China showing shorter operation time, decreased intraoperative blood loss, and better functional outcome but there are no studies assessing the impact on the preoperative plan.
Purpose / Aim of Study: To assess the effect of 3D-printed proximal tibia fractures in the preoperative plan. Secondarily, to perform sub analyses of the effect divided on operative experience.
Materials and Methods: Data on bicondylar proximal tibia fractures treated with open reduction and internal fixation including dual plating was retrieved for 2019. We included 9 consultants in traumatology to do a preoperative plan twice on the basis of CT-scan, thereafter the 3D-print and divided them in to senior (>10 years consultant) and junior (<10 years consultant). Data was entered in an electronic database. We defined an alteration in the preoperative plan as a change in the operative starting point, arthroscopic use, posterior plate, solitary screws, elevation of joint surface through fenestra, and auto-/allograft. Length of plates were also assessed and the surgeons evaluated their confidence after each preoperative plan. Chi-square test was used for categorical group comparison between the 3D- print and the second preoperative plan on the CT-scan.
Findings / Results: There were 9 3D-printed proximal tibia fractures, mean age 60.1 (95% confidence interval, 52.4;67.8), 4 were female and 90% were min. Schatzker type 4. The 3D-print lead to a change in 47% of the preoperative plans with no difference between junior or senior surgeons (p<0.29). The amount of changes was median 1 (1-4). Including changes to the length of plate, there was a change in 81% of the preoperative plans with no differences among the surgeon groups (p<0.512). There was a significant improvement in the level of confidence with the preoperative plan among junior surgeons (p<0.001) but not among senior surgeons (p<0.24).
Conclusions: 3D-print of proximal tibia fractures has a significant effect leading to a change in 47% of the preoperative plans with no difference due to the surgeons’ experience.